CIDP | What Happens Next?
Whether or not someone has been hospitalised, after a diagnosis of CIDP there are still lots of questions regarding what happens next? We hope this section will help answer some of those questions.
Click below to jump to the sections that interests you!
Support and Rehabilitation
If you do need time in hospital, you may require some form of rehabilitation before returning home, to help you regain strength, dexterity and mobility. This could be within a rehabilitation unit in the hospital, or you may be transferred to a specialist rehab unit elsewhere.
You may also be offered psychological support, as a potentially life-changing illness such as CIDP or another chronic inflammatory neuropathy can also severely impact your mental wellbeing.
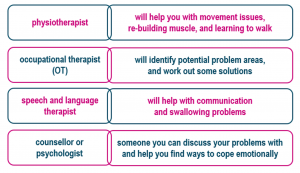
Specialists who might support you through rehab:
General Prognosis
Treatment of CIDP is usually very effective with about 80% of new cases having a dramatic response to therapy. Although some patients go into a long-term remission after a short course of treatment, many require long term treatment as described earlier.
Pregnancy
Neither IVIg nor plasma exchange is contraindicated during pregnancy. However, as plasma exchange requires additional considerations and monitoring, IVIg might be preferred.
Accessing Physiotherapy
If you have difficulty accessing physiotherapy, but feel it would benefit you, or if you find yourself on a lengthy waiting list for community physiotherapy, please contact the office at GAIN.
Hygiene and Cleanliness
Personal cleanliness for those who are unable to attend themselves fully can be a problem. You may have reduced use of your hands, maybe temporarily, but sometimes permanently. Some people may struggle to wash themselves, brush their hair, use the toilet independently, brush their teeth, cut their nails etc. It is important for both hygiene and self-esteem that these matters are attended to by a carer.
Dental Hygiene
Through no fault of their own, many people’s teeth are neglected during periods of serious illness. Once you have returned home, arrange an appointment with your dentist as soon as possible. If you have difficulty attending a dental practice, enquire about community dental services. Using an electric toothbrush can be helpful if you have weakness in your hands. More advice can be found on the British Society for Disability and Oral Health website; https://www.bsdh.org/index.php/how-to-find-a-special-care-dentist
Financial Help
Financial concerns may be causing anxiety, especially if you are the main wage-earner and unable to work. If you are employed, stay in regular contact with employers and make sure you understand the absence and returning to work processes. There is more information about returning to work later in the booklet.
GAIN may be able to help with the cost of frequent journeys to visit a family member in hospital. Visit the website or get in touch and ask about our Personal Grants Scheme.
Once you leave hospital, or if you are already receiving treatment as an outpatient, you could be entitled to benefits to help you support yourself and your family. The benefits system is complex and subject to change, but Citizens Advice has up-to-date information on their website, and they can even help you make an application for benefits such as Personal Independence Payment (PIP) or Universal Credit: https://www.citizensadvice.org.uk/
Further information on benefits can be found at https://www.gov.uk/browse/benefits
If adaptations to your home are needed, such as installing a ramp or downstairs bathroom for example, it is worth contacting your local council to see if you are entitled to help via a Disabled Facilities Grant:
England and Wales
https://www.gov.uk/apply-disabled-facilities-grant
Scotland
http://www.disabilityscot.org.uk/info-guides/disabled-home-adaptations-1/
Northern Ireland
https://www.nidirect.gov.uk/articles/disabled-facilities-grants-0
Republic of Ireland https://www.citizensinformation.ie/en/housing/housing_grants_and_schemes/housing_adaptation_grant_for_people_with_disability.html
If you are on a low income, or someone in your household is severely and permanently disabled, you may be entitled to a reduction in Council Tax. Further information is available in the Carers UK Council Tax factsheet: https://www.carersuk.org/images//Factsheets/2020-21_factsheets/Council_Tax_April_2020-21.pdf
Your Immune System
Although caused by your immune system malfunctioning, CIDP does not weaken or damage your immune system, and having CIDP does not mean that your immune system is compromised, unless you are being treated with steroids.
Regular exercise and maintaining a healthy diet and sleep regime will all help during recovery. There is anecdotal evidence, and lots of hype surrounding supplements and alternative remedies, but very few are known to have real benefits. Most people are able to get the vitamins they need from their diet, but if you wish to take dietary supplements, your doctor (rather than Google!) will be able to advise you on anything that may help you during recovery.
Diet
During illness, nutritional needs are at their peak, but it is not unusual for patients to lose their appetites or taste for food. Worry and fear often accompany illness and can also contribute to loss of appetite. Good nutrition can be a powerful ally in the process of recovery, so if you need advice, ask to speak to a nutritionist. If taste has been affected, this will usually improve with time. Plastic utensils can be used if bitter or metallic tastes are experienced whilst eating. Sometimes taste changes can be related to medications, but drugs should not be discontinued without first consulting your GP. Try to eat a healthy, balanced diet and keep consumption of sugary and processed foods, and drinks that are high in caffeine or alcohol to a minimum. There is some excellent advice on nutrition on the NHS website; https://www.nhs.uk/live-well/eat-well/
Exercise and Rest
Physiotherapy, occupational therapy (OT) and speech and language therapy play a vital role in maximizing functional ability.
Exercise can help to improve your muscle strength and reduce your overall sense of fatigue. It can also aid sleep and support mood through the production of endorphins. Other benefits include helping your heart and lungs remain healthy and making you feel more positive about yourself. However, it may take weeks or even months before you feel some of the benefits, so it is important to pace yourself. You will find lots of exercises online, including seated exercises, or you could ask your GP or physiotherapist about how to start regular exercise and what exercises might be right for you.
Visit the NHS website for advice on exercise: https://www.nhs.uk/live-well/exercise/
and also for advice on sleep: https://www.nhs.uk/live-well/sleep-and-tiredness/
Pain
Being in pain naturally impacts on mood and the ability to cope with everyday situations. If you are experiencing pain, it is important to talk to your family and friends about this, so that they understand what you are going through and why you might be irritable and difficult to live with at times.
Some other sources of support are shown below.
|
Other sources of support PAIN
|
|
| Pain Concern |
|
| British Pain Society |
https://www.britishpainsociety.org/
|
|
Pain Association Scotland
|
https://painassociation.co.uk/ |
| Welsh Pain Society |
https://www.welshpainsociety.org.uk/
|
| Pain Relief Foundation |
https://painrelieffoundation.org.uk/
|
| Pain Management NI |
https://www.myni.life/pain-management
|
| Pain Relief Ireland |
|
Welcome to our CIDP Information Hub.
Here we breakdown what is happening to you or a loved in simple but proper terms. Our information is sourced from our Medical Advisory Board, medical texts, and recognised support providers.
If you have any questions after reading this that you feel haven’t been answered. Please get in touch with us, we will strive to point you in the right direction.
What is CIDP?
We discuss the basics of GBS – what it is, the symptoms, and information on Acute onset CIDP (A-CIDP)
How is CIDP Treated?
We cover Immunoglobulin, Plasma Exchange, Corticosteroids, and is there a “cure”?
What Family & Friends Can Do To Help if Someone is in Hospital?
We cover communication, Mental Stimulation, Financial Worries, Comfort, Coming off a Ventilator, and Staying Positive
What is the advice surrounding vaccinations and CIDP?
Containing information on vaccinations via our Medical Advisory Board and sourced journals.
Mental Health & Wellbeing, Relationships, and Carer Support
Contains information on how to care for your mental health. We also discuss relationships, before a section on looking after yourself as a carer
What Are The Causes of CIDP?
How will I get diagnosed by my Doctor, Nerve Tests, and Lumbar Punctures
Returning to Work
When someone is ready to return to work after an absence, the employer should have a procedure they follow.
You can check your workplace’s absence policy for this. Your workplace might have a policy for meeting with employees after absences.











