What family and friends can do to help when someone is in hospital
Click below to quickly access the topic you’re most interested in!
Communication
Understand as much as you can about this condition. If you are the person visiting most frequently, introduce yourself to the doctor in charge of the case and don’t be afraid to ask questions. Some doctors are better than others at explaining things, so let them know if you don’t understand. Get to know the regular nursing staff and ask for a daily update on progress.
Physiotherapy can start while the patient is still paralysed. Get to know the physio and keep yourself updated on procedure and progress. They can tell you how you can help with exercises between physio sessions.
Talk to the speech therapist about communication aids. If facial muscles aren’t paralysed, then lip reading could help. Some people retain finger movement and can write letters in the air or on the palm of the hand. A common method of communication with a patient whose movements are restricted to the eyes and eyelids, is to use a question and answer technique with the patient answering with one blink for ‘yes’ and two for ‘no’. Pointing to the letters on an alphabet board and asking ‘Is it on this line? Is this the letter?’, will help. If the patient is strong enough, they may be able to point at an alphabet board with a finger or pointer attached to a headband.
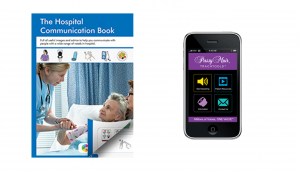
A hospital communication book contains lots of words and images useful in a hospital setting and can pre-empt many questions or comments a ventilated patient is likely to make. GAIN will send you a free copy on request, that you can leave at the bedside for staff and visitors to use.
Another useful tool is an app developed by David Muir, who was ventilated due to muscular dystrophy and became non-verbal as a result. The app is called Passy Muir Trachtools and is free to download in your app store for Apple and android devices. It has several pre-recorded phrases, and allows you to record your own customized words and messages. When you find a communication method that works, make sure you share this with staff and other visitors so they can adopt the same practice.
Mental Stimulation
Remember they are socially isolated and will need to be stimulated. Tell them what day it is and talk about what is happening in the outside world. Read extracts from a national or local newspaper and encourage friends and family to send cards and texts about what they are up to. Remember to include them in all conversations, even if they can’t respond verbally.
Make use of your tech! Read to them or offer to play an audio book on their smartphone or tablet. Download films, favourite TV shows and music onto their device and watch or listen together if you can, with one earbud each.
Financial Worries
Financial concerns may be causing anxiety, especially if the patient is the main wage-earner. Get in touch with the Social Worker at the hospital who will advise on benefits. Alternatively, Citizens’ Advice offers free expert advice which you access online, or by phoning your local office. Stay in regular contact with employers and make sure you understand the absence and returning to work processes. There is more information about returning to work later in the booklet.
GAIN may be able to help through our Personal Grants Scheme with travel costs for frequent journeys visiting a family member in hospital.
Comfort
The little things you can do will mean a lot. Do they need a hair wash or a shave? Do nails need manicuring? Can you help by massaging their hands or feet? Eating and drinking while you’re visiting might have a negative impact, if they are unable to swallow anything, so make sure you have something before you arrive.
Some patients have pain in the acute stage, others as recovery kicks in, and some have no pain at all. Try to understand what pain they have, if any, and the frequency and type of medication being given to alleviate it.
GBS patients tire easily, may be on sedative drugs and tend to nap quite frequently. They might not want visitors over and above one or two close family members, especially in the early stages following diagnosis and the start of recovery.
At the end of your visit, make sure you leave them in the best possible frame of mind. Turn off any device that might cause irritation or disturbance and make sure they have what they need or can attract attention if required.
Coming off the Ventilator
As things improve, they will be taken off the ventilator, often starting with just a few minutes and building up gradually. Patients can get quite panicky at the beginning of this procedure as they have become reliant on the ventilator and might not believe that they can breathe again without it. Reassure them that their natural ability to breathe is returning and that this is the start of getting well.
Once off the ventilator, it is likely that they will soon be transferred to a general ward for a time before moving into a rehab unit or being discharged home. Moving out of ICU, where patients are monitored continuously, can be stressful in itself, but it’s all part of recovery, and no one will be moved until the medical team is satisfied that they are ready.
Stay Positive
Your role is to offer love, comfort and reassurance during this difficult period. Try to remain calm and positive and give lots of encouragement on progress. Keep yourself well informed by the medical staff. Writing a few lines each day in a journal will help you keep a perspective on progress. You can share this over the coming weeks to show how far they’ve come since those early days. For close family, this period of the illness can be an exhausting time of stress, uncertainty and disruption, as you struggle to maintain other commitments alongside frequent hospital visits, so don’t forget to look after yourself and stay well.
Welcome to our CIDP Information Hub.
Here we breakdown what is happening to you or a loved in simple but proper terms. Our information is sourced from our Medical Advisory Board, medical texts, and recognised support providers.
If you have any questions after reading this that you feel haven’t been answered. Please get in touch with us, we will strive to point you in the right direction.
What is CIDP?
We discuss the basics of GBS – what it is, the symptoms, and information on Acute onset CIDP (A-CIDP)
How is CIDP Treated?
We cover Immunoglobulin, Plasma Exchange, Corticosteroids, and is there a “cure”?
What Family & Friends Can Do To Help if Someone is in Hospital?
We cover communication, Mental Stimulation, Financial Worries, Comfort, Coming off a Ventilator, and Staying Positive
What is the advice surrounding vaccinations and CIDP?
Containing information on vaccinations via our Medical Advisory Board and sourced journals.
Mental Health & Wellbeing, Relationships, and Carer Support
Contains information on how to care for your mental health. We also discuss relationships, before a section on looking after yourself as a carer
What Are The Causes of CIDP?
How will I get diagnosed by my Doctor, Nerve Tests, and Lumbar Punctures
Returning to Work
When someone is ready to return to work after an absence, the employer should have a procedure they follow.
You can check your workplace’s absence policy for this. Your workplace might have a policy for meeting with employees after absences.











