CIDP and associated chronic inflammatory neuropathies
Introduction
The peripheral nerves are made of bundles of nerve fibres, which can be regarded as living telephone wires. They are kept alive by their cell bodies. The cell bodies of the motor nerves lie in the spinal cord within the spinal column or around the base of the brain. The cell bodies of the sensory nerves are in bunches, called ganglia, connected to the nerve roots on the back of the spinal cord or brain stem.
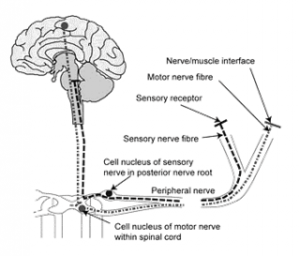
The motor nerve cell body has a long fibre called an axon, which extends from the central nervous system to the muscles. The longest axons can be as much as a metre in length, for example the nerves to the muscles in the feet. The connection between the motor axon and the muscle fibre is a specialised nerve ending, which contains tiny packets of a chemical. The motor nerve stimulates the motor nerve ending to release the chemical and make the muscle fibre contract. If a peripheral neuropathy affects the motor nerves, the muscles become weak because they do not receive the messages to move.
The cell body of a sensory nerve has two axons. One goes into the spinal cord and delivers messages to the brain. The other come from specialised receptors in the skin, joints and muscles and transmits messages from them. The receptors sense changes in pressure, position, or temperature or pain. The receptor translates the stimulus into a nerve impulse. The sensory nerve fibres relay the impulses to the brain.
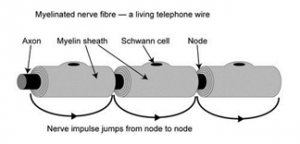
The fastest conducting nerve fibres are like telephone wires and have their own insulating sheaths. The sheaths are made of myelin, a fatty substance made by special cells, called Schwann cells. Nerve fibres conduct nerve impulses very quickly because the myelin sheath has gaps about every milimetre, which allow the nerve impulse to jump from gap to gap and travel faster. These fast conducting myelinated nerve fibres control rapid movement and allow fine touch discrimination. There are also many nerve fibres without myelin sheaths. These are called unmyelinated fibres and conduct nerve impulses more slowly. They signal pain and temperature and are important for the control of blood circulation and sweating.
Different types of peripheral neuropathy
Most types of peripheral neuropathy usually come on very slowly over several months or years, a clinical course called chronic. Sometimes a peripheral neuropathy comes on very rapidly over the course of a few days, which is called acute. Intermediate courses, about four to eight weeks, are called subacute.
A peripheral neuropathy often affects all the nerves more or less together. Because the longest nerves are the most vulnerable, the feet and then the hands are most affected. Such a symmetrical pattern, affecting the feet and hands more than the hips and shoulders, is called a symmetrical polyneuropathy (poly means many). If only one nerve is affected, the condition is called a mononeuropathy (mono means single). If several discrete nerves are affected, the condition is called a multiple mononeuropathy (the term ‘mononeuritis multiplex’ might also be used). Sometimes the nerve roots (the name for parts of the nerves next to the spinal cord) are also affected, which gives rise to a polyradiculoneuropathy (radiculo means root). Polyradiculoneuropathy occurs in the common form of Guillain-Barré syndrome (GBS) and in chronic inflammatory demyelinating polyradiculoneuropathy (CIDP).
A peripheral neuropathy usually affects sensory and motor nerve fibres together so as to cause a mixed sensory and motor neuropathy. Sometimes the autonomic nerve fibres are also affected. These control sweating, pulse, blood pressure, bladder, sexual and bowel function which may become affected. Sometimes a peripheral neuropathy just affects sensory nerve fibres, causing a pure sensory neuropathy. Finally the motor nerve fibres may be affected on their own, producing a pure motor neuropathy.
Nerve fibres may be damaged in four main ways:
- Most commonly, the delicate long axons lose their energy supply because of a chemical upset in the nerve cell body causing the axon to This is called an axonal neuropathy.
- Less commonly the problem lies in the insulating myelin This is called a demyelinating neuropathy.
- Vasculitis(inflammation of the blood vessels) may affect the nerves and cause a vasculitic
- Sometimes unusual chemicals or cells collect in the nerves and cause an infiltrative
Peripheral neuropathies do not affect the brain, vision, or the sense of smell. They almost never affect hearing and taste. Most sorts of peripheral neuropathy do not affect breathing or swallowing.
What is CIDP?
Chronic inflammatory demyelinating poly-radiculo-neuropathy (CIDP) is a neurological disorder characterized by progressive weakness and impaired sensory function in the legs and arms. The disorder, which is sometimes called chronic relapsing polyneuropathy, is caused by damage to the myelin sheath (the fatty covering that wraps around and protects nerve fibres) of the peripheral nerves. You need to have had symptoms for at least 8 weeks for CIDP to be considered. Although it can occur at any age and in both genders, CIDP is more common in young adults, and in men more so than women.
The course of CIDP varies widely among individuals. Some may have a bout of CIDP followed by spontaneous recovery, while others may have many bouts with partial recovery in between relapses. The disease is a treatable cause of acquired neuropathy and initiation of early treatment to prevent loss of nerve axons is recommended. However, some individuals are left with some residual numbness or weakness, and abnormal sensations. CIDP is closely related to Guillain-Barre syndrome and it is considered the chronic counterpart of that acute disease.
Symptoms of CIDP
Symptoms of CIDP usually develop slowly starting in the feet and legs before progressing to other parts of the body. The symptoms experienced vary considerably between patients and may be vague and confusing to both the patient and the doctor. Subjective symptoms such as fatigue and sensory disturbance are difficult to communicate.
These symptoms may remain mild and result in only minor disruption of the patent’s normal life. Alternatively, they may become progressive and gradually worse over a period of several weeks, months or even years — sometimes but very rarely, to the extent that the patient is bed bound with profound weakness of the arms.

Acute onset CIDP (A-CIDP)
Due to similarity in the early stages up to 16% of patients will be misdiagnosed with GBS (AIDP), meaning patients may not receive the best treatment for their condition or understand the long-term outcomes.
Patients with A-CIDP are less likely to have autonomic nervous system involvement, facial weakness, a preceding infectious illness, or the need for mechanical ventilation. Around 8%-16% of GBS patients may relapse shortly after improvement or stabilization following initial immunological therapy. This is an important clinical issue because maintenance treatment is often required in CIDP. The diagnosis of A-CIDP should be considered when the condition of a patient with GBS deteriorates after nine weeks from onset, or when deterioration occurs three times or more.
What causes CIDP?
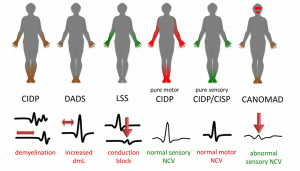
Pattern of symptoms in chronic conditions
Although sometimes a trigger is apparent, and in contrast to GBS, most patients with CIDP cannot identify a preceding viral or bacterial infection. GBS normally progresses over 2-4 weeks, then plateaus, improves over several months and does not usually recur. CIDP has ongoing symptoms for over 8 weeks and usually does not improve unless ongoing treatment is given.
How is CIDP diagnosed?
CIDP can be difficult to diagnose as there is no single, conclusive diagnostic test for it. The symptoms are often vague and can be produced by a number of different conditions. Therefore, a long period of time may elapse before a diagnosis of CIDP is made. A diagnosis of CIDP requires the following:
• weakness of at least two limbs
• complete or partial loss of tendon reflexes
• progression or relapse eight weeks or more after initial disease onset
• evidence of myelin damage in the peripheral nerves from nerve conduction studies
A diagnosis of CIDP is usually made on clinical grounds but with evidence from:
• nerve conduction studies
• lumbar puncture
• MRI scan
• nerve biopsy
• ruling out other diseases that can cause demyelinating neuropathy
• family history to completely rule out an inherited neuropathy
• contact with possible toxins or drugs that could cause neuropathy
• other conditions – diabetes, alcohol dependency, arthritis or hepatitis
Nerve Tests
In hospital, two tests may be carried out to see how well your nerves are working. These are
• electromyogram (EMG) – tiny needles are inserted into your muscles and electrical recordings are taken to see how they react when nearby nerves are activated.
• nerve conduction studies – small discs (electrodes) are stuck on your skin and minor electric shocks are used to activate the nerves and measure how quickly these signals travel along them.
In people with GBS, these tests will usually show that signals are not travelling along the nerves properly.
Lumbar Puncture
The lumbar puncture is a procedure to remove some fluid from around the spinal cord (the nerves running up the spine) which involves lying on one side and having a needle inserted into the base of the spine under local anesthetic.
The sample of fluid will be checked for signs of problems that can cause similar symptoms to GBS, such as an infection.
Occasionally the diagnosis can be delayed for a few days while they are checking the results, and your doctor may start the treatment just to be on the safe side.
Treatment
The treatments with clinically proven efficacy in CIDP are immunoglobulin, steroids, and plasma exchange, all of which have been shown to be superior to placebo in clinical trials. In other studies, they have been shown to be equivalent to one another in efficacy: between 50 and 80% of patients respond to each of the treatments. Failure to respond to one treatment does not mean that the other treatments won’t work either (unless the diagnosis if wrong). 15% of patients do not respond to any of the three treatments.
Immunoglobulin
The most commonly used treatment, particularly for motor dominant CIDP, is intravenous immunoglobulin (IVIg). Immunoglobulin is made from donated blood that contains healthy antibodies which can help stop the harmful antibodies damaging your nerves. If it works there will be a quick response in a matter of weeks, with improvement in strength and function. Some patients (15-30%) only need a single course.
IVIg is given in hospital and if it needs to be given long term by regular infusion typically every 6 weeks. This can have an impact on the patient’s work, travel plans, or ability to look after family members, as their infusions need to be fitted around these factors.
In some parts of the country it is possible to receive subcutaneous immunoglobulin (also known as SCIg or SubCut) at home which is more convenient for patients. With SCIg, immunoglobulin is delivered by a needle into the fatty tissues under the skin, where it enters the circulation slowly over a few days. There isn’t much room under the skin, so the dose of immunoglobulin given is smaller than with IVIg. For this reason, SCIg is usually given every week. Nearly everybody on SCIg learns how to have treatment at home, with each session lasting up to about two hours.
As with all treatments, side effects can occur with IVIg, although usually these are minimal and do not require the treatment to be stopped. It is helpful if you drink plenty of fluid whilst you are receiving IVIg. Transient side effects, which often respond to changes in the rate of administration of the infusion, include headache and low blood pressure and occasionally, a rash can develop. Severe complications from IVIg use are very rare. IVIg thickens the blood slightly so particular consideration of its use is given to patients with kidney failure, previous heart disease, stroke or blood clots.
Plasma Exchange (plasmapheresis)
Plasma exchange, also called plasmapheresis, is sometimes used instead of IVIg. This involves being attached to a machine that removes blood from a vein and filters out the harmful antibodies that are attacking your Plasma exchange involves having the patient attached to a machine to remove some of their blood and replace with other blood product (eg human albumin), over 5 days. PE should be considered in preference to IVIg in cases of non-motor dominant CIDP.
Corticosteroids
Corticosteroids should also be considered in preference to IVIg in cases of non-motor dominant CIDP. Corticosteroids are easy to administer either as daily or alternate daily treatments, or monthly oral or intravenous regimes. In older patients, there are often competing medical conditions which mean that they need to be used with caution or avoided altogether e.g. if a patient has poorly controlled diabetes or osteoporosis, or if they have recurrent chest infections and immunosuppression might put them at risk of overwhelming infection. A younger patient may have fewer comorbidities but would also potentially be facing longer term treatment.
If a patient needs very frequent IVIg infusions then a neurologist might consider adding in a steroid or another immunosuppressant agent, and if IVIg does not offer clear benefits, then steroids are the obvious next treatment option. There is a difference in cost between the treatment options, with both IVIg and plasma exchange costing thousands of pounds per course whilst steroids are relatively cheap, but this is not a deciding factor in which treatment is provided.
Is there a cure for CIDP?
It depends how you define ‘cure’, but in CIDP literature this has been defined as ‘remission of over 5 years off treatment’, which has been reported in about 25% of patients treated with steroids for less than one year. Neurologists would more usually use the term ‘remission’ in CIDP (i.e. stability without treatment). Shorter term remission is more common than ‘cure’: there is evidence from studies that up to 40% of patients with CIDP may be in remission after one year of treatment with either steroids or IVIg. It is for this reason that it is advised that the need for treatment is reviewed on an annual basis if patients are no longer showing any or little fluctuation in their clinical symptoms. Although many people remain free of symptoms following remission, there is no guarantee that there will be no further relapse in the future. 15% of patients do not respond to any of the three treatments.
Other Chronic Conditions
Paraproteinaemic Demyelinating Neuropathy (PDN)
Sometimes described as:
- chronic demyelinating neuropathy associated with a benign paraprotein
- CIDP associated with paraprotein
- CIDP with paraproteinaemia
Antibody-producing bone marrow cells go out of control and produce large numbers of the same antibody. The antibody (or immunoglobulin) sometimes damages nerve fibres causing a peripheral neuropathy. Some doctors regard the clinical, electrophysiological and pathological features of the demyelinating paraproteinaemic neuropathies and of CIDP as closely similar and almost indistinguishable.
These neuropathies are usually late-onset in terms of age and are mixed motor and sensory, although the severity of sensory loss tends to be greater compared with CIDP. There is usually more pain but less severe weakness and impairment. Most patients respond to corticosteroids, cytotoxic drugs, or plasma exchange.
Multifocal Motor Neuropathy (MMN)
or MMN with Conduction Block (MMNCB)
Sometimes thought of as a rare variant of CIDP. However, there are differences that are more prominent than the similarities. MMN patients commonly have asymmetric weakness of the distal (far) muscles, while in CIDP, proximal (near) symmetric weakness is more common. The remitting and relapsing course that may occur in CIDP is uncommon in MMN. Patients with MMN rarely have significant sensory symptoms, unlike CIDP. Increased protein level in the cerebrospinal fluid of MMN patients is rare. Treatment with IVIg or cyclophosphamide is usually effective.
MADSAM also known as Lewis-Sumner syndrome
Multifocal acquired demyelinating sensory and motor neuropathy is a chronic condition with similarities to multifocal motor neuropathy but with enough differences, especially in treatment, to have acquired its own definition. Some report it to be an asymmetrical variant of CIDP. MMN and MADSAM respond to IVIg. Some MADSAM sufferers respond to prednisolone whilst most MMN sufferers do not.
Chronic axonal neuropathies are common, particularly as a result of diabetes or alcoholism. However, the medical literature does report cases of immune-mediated chronic axonal neuropathy though there are suggestions that this is a secondary result of myelin damage that ultimately appears to be the primary cause of the condition.
Sub-acute Inflammatory Demyelinating Poly(radiculo)neuropathy (SIDP) GBS is defined when the nadir (worst point) occurs within four weeks of first symptoms, and CIDP is defined when the nadir comes after at least eight weeks. An illness peaking after four weeks but before eight weeks may be called subacute and will be treated as CIDP or GBS depending on which it best resembles.
Chronic idiopathic axonal neuropathy
If no cause for the peripheral neuropathy can be discovered, doctors call it ‘idiopathic’ that means ‘of its own cause’. This label probably covers a number of different causes which future research may uncover. With rare exceptions, chronic idiopathic axonal neuropathy occurs in older people, only worsens very slowly (and sometimes remains stationary), and does not become disabling. It is most commonly a sensory neuropathy causing numbness, tingling and discomfort in the feet that may gradually spread up the shins.
People may become slightly unsteady, and weakness of the ankles may develop. The amount of pain is variable. Some people have very little pain but more weakness. Others have little weakness but more pain.
Sensory neuronopathy
Also known as sensory ganglionopathy, dorsal root ganglionopathy or sensory ganglionopathy, this is a rare subgroup of peripheral nervous system diseases with specific characteristics, such as the primary and selective destruction of the dorsal root ganglia (DRG) neuron in the spinal cord and the trigeminal ganglia neuron in the skull.
It has a typical clinical presentation, with sensory deficits that are not dependent on length and patients often report a lack of coordination of muscle movements. There are several proposed mechanisms for the pathophysiology of the condition. The diagnosis is guided by the presenting symptoms and confirmed with diagnostic tests to differentiate from other related conditions.
Treatment of sensory ganglionopathy is often difficult and patients often stabilize but fail to improve significantly. There are reports of improvement in immune-mediated and paraneoplastic sensory ganglionopathy following treatment with intravenous immunoglobulin and rituximab, respectively. Quickly treating the underlying cause, such as the underlying neoplasia, may also be helpful.
Related Conditions
People that suffer from sensory neuronopathy are more likely to be affected by other autoimmune diseases. A differential diagnosis is important to distinguish sensory neuronopathy from other related conditions, such as sensory and ataxic neuropathy. These conditions may include Sjögren’s Syndrome, autoimmune hepatitis and celiac disease.
POEMS syndrome
POEMS is a rare condition caused by the body producing abnormal plasma cells (a type of blood cell which produces antibodies to fight off infections). This blood disorder affects multiple organs in the body. It is named after the five common features of the syndrome described below.
Polyneuropathy – nerve damage leading to weakness, numbness and pain in the arms and legs
Organomegaly – an enlarged spleen and/or liver
Endocrinopathy – hormonal problems
M-protein or Monoclonal plasma cell disorder – an overproduction of abnormal plasma cells which lead to other multi system effects
Skin changes – darkening to skin, red spots on the body, hair growth
For more information, please see our POEMS fact sheet click here
Living with CIDP
Not everyone with CIDP will require a stay in hospital, but if CIDP comes on very rapidly, presenting more like GBS, it may be necessary to be admitted to ICU for a time. As this won’t apply to them majority of people diagnosed with CIDP, more information about ICU is available on a separate information sheet.
If you do require a stay in hospital, you’ll be closely monitored to check for any problems with your lungs, heart or other body functions. You’ll also be given treatment to relieve your symptoms and reduce the risk of further problems. This may include:
- a ventilator if you’re having difficulty breathing
- a feeding tube if you have swallowing problems
- painkillers if you’re in pain
- being gently moved around on a regular basis to avoid bed sores and keep your joints healthy
- a thin tube called a catheter in your urethra (the tube that carries urine out of the body) if you have difficulty peeing
- laxatives if you have constipation
- medicine and/or special leg stockings to prevent blood clots
Once you start to improve, you may also need extra support to aid your recovery.
Depending on the severity of symptoms, and how well they respond to treatment, you may need help with everyday tasks, your home may need adaptations, or you may need a care package in place.
Support and rehabilitation
If you do need time in hospital, you may require some form of rehabilitation before returning home, to help you regain strength, dexterity and mobility. This could be within a rehabilitation unit in the hospital, or you may be transferred to a specialist rehab unit elsewhere.
You may also be offered psychological support, as a potentially life-changing illness such as CIDP or another chronic inflammatory neuropathy can also severely impact your mental wellbeing.
General prognosis
Treatment of CIDP is usually very effective with about 80% of new cases having a dramatic response to therapy. Although some patients go into a long-term remission after a short course of treatment, many require long term treatment of one form or another. Drug treatments are generally thought to work by suppressing the autoimmune response, which in turn reduces the disabling symptoms of the disease.
Vaccinations
Vaccines in CIDP
Professor Michael Lunn MA MBBS FRCP PhD, Consultant Neurologist and Professor of Clinical Neurology, National Hospital for Neurology and Neurosurgery, Queen Square, London advises: “One vaccine is not the same as another. The only reason that one advises against flu vaccine in someone with GBS is if they actually had GBS in the 6 week window after a flu vaccine and then only out of an abundance of caution which is not based on any real science. The rate of GBS after flu vaccine in all assessed years after 1976 has been about 1 per million and no study has linked vaccination to recurrence of GBS or CIDP. COVID vaccine is nothing like flu vaccine. Although there have been a small number of people who have developed GBS for the first time following the COVID vaccine, the risk of serious illness and complications from COVID are greater.”
None of the COVID vaccines approved to date is live attenuated, but should a live vaccine become available, then this should be avoided by anyone whose immune system is suppressed, due to taking corticosteroids to treat CIDP for example.
Most people don’t need a flu jab. However, if you are in an at-risk group, or you live or work closely with people for whom flu might be severe or life-threatening, then you should be vaccinated, to protect yourself and others.
On vaccinations in general, our Medical Advisory Board advises:
- DON’T have unnecessary vaccines for travel but DO have all travel vaccines that are recommended for the particular area you are travelling to.
- DO have all vaccines that are ‘necessary’. This includes the flu vaccine (if you are in an at risk group), MMR, DTP, pneumovax, HIF, COVID-19, etc. There are monitoring programmes ongoing so a link would be picked up if it occurred.
- COVID-19 is a more serious disease than influenza and more easily caught. Most people with GBS or CIDP should receive any of the COVID-19 vaccines, except perhaps people with a history of severe allergy requiring an Epipen.
Vaccines currently in use are amongst the safest medicines available. However, there is no simple ‘yes or no’ answer, and each person must weigh up the risks of not having a vaccination against the very small possible risk from having it.
Having relatively mild side effects such as numbness and tingling is quite common following a vaccination, and is almost certainly nothing to be concerned about. If you have had GBS in the past, or if you have an associated chronic neuropathy such as CIDP, a vaccination might cause a slight ‘flare-up’ of symptoms due to your immune system being stimulated. Most will only last a few days, but if they last longer than this, or if symptoms get worse or start spreading, then I would suggest contacting your GP. Anyone can report side effects of medication or vaccines, regardless of severity, and if you would like to do so, please follow this link; https://coronavirus-yellowcard.mhra.gov.uk/
1Jeffrey C. Kwong, Priya P. Vasa, Michael A. Campitelli, Steven Hawken, Kumanan Wilson, Laura C. Rosella, Therese A. Stukel, Natasha S. Crowcroft, Allison J. McGeer, Lorne Zinman and Shelley L. Deeks The risk of Guillain-Barré Syndrome following seasonal influenza vaccination and influenza healthcare encounters, a self-controlled study. The Lancet Infectious Diseases, Vol. 13, No. 9, p730–731 Published: June 28, 2013
2Chen, Y., Zhang, J., Chu, X. et al. Vaccines and the risk of Guillain-Barré syndrome. Eur J Epidemiol 35, 363–370 (2020).
What family and friends can do to help
Communication
Understand as much as you can about this condition. If you are the person visiting most frequently, introduce yourself to the doctor in charge of the case and don’t be afraid to ask questions. Some doctors are better than others at explaining things, so let them know if you don’t understand. Get to know the regular nursing staff and ask for a daily update on progress.
Physiotherapy can start while the patient is still paralysed. Get to know the physio and keep yourself updated on procedure and progress. They can tell you how you can help with exercises between physio sessions.
Talk to the speech therapist about communication aids. If facial muscles aren’t paralysed, then lip reading could help. Some people retain finger movement and can write letters in the air or on the palm of the hand. A common method of communication with a patient whose movements are restricted to the eyes and eyelids, is to use a question and answer technique with the patient answering with one blink for ‘yes’ and two for ‘no’. Pointing to the letters on an alphabet board and asking ‘Is it on this line? Is this the letter?’, will help. If the patient is strong enough, they may be able to point at an alphabet board with a finger or pointer attached to a headband.
A hospital communication book contains lots of words and images useful in a hospital setting and can pre-empt many questions or comments a ventilated patient is likely to make. GAIN will send you a free copy on request, that you can leave at the bedside for staff and visitors to use.
Another useful tool is an app developed by David Muir, who was ventilated due to muscular dystrophy and became non-verbal as a result. The app is called Passy Muir Trachtools and is free to download in your app store for Apple and android devices. It has several pre-recorded phrases, and allows you to record your own customized words and messages. When you find a communication method that works, make sure you share this with staff and other visitors so they can adopt the same practice.
Mental stimulation
Remember they are socially isolated and will need to be stimulated. Tell them what day it is and talk about what is happening in the outside world. Read extracts from a national or local newspaper and encourage friends and family to send cards and texts about what they are up to. Remember to include them in all conversations, even if they can’t respond verbally.
Make use of your tech! Read to them or offer to play an audio book on their smartphone or tablet. Download films, favourite TV shows and music onto their device and watch or listen together if you can, with one earbud each.
Financial worries
Financial concerns may be causing anxiety, especially if the patient is the main wage-earner. Get in touch with the Social Worker at the hospital who will advise on benefits. Alternatively, Citizens’ Advice offers free expert advice which you access online, or by phoning your local office. Stay in regular contact with employers and make sure you understand the absence and returning to work processes. There is more information about returning to work later in the booklet.
GAIN may be able to help through our Personal Grants Scheme with travel costs for frequent journeys visiting a family member in hospital.
Comfort
The little things you can do will mean a lot. Do they need a hair wash or a shave? Do nails need manicuring? Can you help by massaging their hands or feet? Eating and drinking while you’re visiting might have a negative impact, if they are unable to swallow anything, so make sure you have something before you arrive.
Some patients have pain in the acute stage, others as recovery kicks in, and some have no pain at all. Try to understand what pain they have, if any, and the frequency and type of medication being given to alleviate it.
GBS patients tire easily, may be on sedative drugs and tend to nap quite frequently. They might not want visitors over and above one or two close family members, especially in the early stages following diagnosis and the start of recovery.
At the end of your visit, make sure you leave them in the best possible frame of mind. Turn off any device that might cause irritation or disturbance and make sure they have what they need or can attract attention if required.
Coming off the ventilator
As things improve, they will be taken off the ventilator, often starting with just a few minutes and building up gradually. Patients can get quite panicky at the beginning of this procedure as they have become reliant on the ventilator and might not believe that they can breathe again without it. Reassure them that their natural ability to breathe is returning and that this is the start of getting well.
Once off the ventilator, it is likely that they will soon be transferred to a general ward for a time before moving into a rehab unit or being discharged home. Moving out of ICU, where patients are monitored continuously, can be stressful in itself, but it’s all part of recovery, and no one will be moved until the medical team is satisfied that they are ready.
Stay positive
Your role is to offer love, comfort and reassurance during this difficult period. Try to remain calm and positive and give lots of encouragement on progress. Keep yourself well informed by the medical staff. Writing a few lines each day in a journal will help you keep a perspective on progress. You can share this over the coming weeks to show how far they’ve come since those early days. For close family, this period of the illness can be an exhausting time of stress, uncertainty and disruption, as you struggle to maintain other commitments alongside frequent hospital visits, so don’t forget to look after yourself and stay well.
What happens next
Support and rehabilitation
If you do need time in hospital, you may require some form of rehabilitation before returning home, to help you regain strength, dexterity and mobility. This could be within a rehabilitation unit in the hospital, or you may be transferred to a specialist rehab unit elsewhere.
You may also be offered psychological support, as a potentially life-changing illness such as CIDP or another chronic inflammatory neuropathy can also severely impact your mental wellbeing.
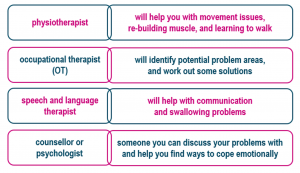
Specialists who might support you through rehab:
General prognosis
Treatment of CIDP is usually very effective with about 80% of new cases having a dramatic response to therapy. Although some patients go into a long-term remission after a short course of treatment, many require long term treatment as described earlier.
Pregnancy
Neither IVIg nor plasma exchange is contraindicated during pregnancy. However, as plasma exchange requires additional considerations and monitoring, IVIg might be preferred.
Accessing physiotherapy
If you have difficulty accessing physiotherapy, but feel it would benefit you, or if you find yourself on a lengthy waiting list for community physiotherapy, please contact the office at GAIN.
Hygiene and cleanliness
Personal cleanliness for those who are unable to attend themselves fully can be a problem. You may have reduced use of your hands, maybe temporarily, but sometimes permanently. Some people may struggle to wash themselves, brush their hair, use the toilet independently, brush their teeth, cut their nails etc. It is important for both hygiene and self-esteem that these matters are attended to by a carer.
Dental hygiene
Through no fault of their own, many people’s teeth are neglected during periods of serious illness. Once you have returned home, arrange an appointment with your dentist as soon as possible. If you have difficulty attending a dental practice, enquire about community dental services. Using an electric toothbrush can be helpful if you have weakness in your hands. More advice can be found on the British Society for Disability and Oral Health website; https://www.bsdh.org/index.php/how-to-find-a-special-care-dentist
Financial help
Financial concerns may be causing anxiety, especially if you are the main wage-earner and unable to work. If you are employed, stay in regular contact with employers and make sure you understand the absence and returning to work processes. There is more information about returning to work later in the booklet.
GAIN may be able to help with the cost of frequent journeys to visit a family member in hospital. Visit the website or get in touch and ask about our Personal Grants Scheme.
Once you leave hospital, or if you are already receiving treatment as an outpatient, you could be entitled to benefits to help you support yourself and your family. The benefits system is complex and subject to change, but Citizens Advice has up-to-date information on their website, and they can even help you make an application for benefits such as Personal Independence Payment (PIP) or Universal Credit: https://www.citizensadvice.org.uk/
Further information on benefits can be found at https://www.gov.uk/browse/benefits
If adaptations to your home are needed, such as installing a ramp or downstairs bathroom for example, it is worth contacting your local council to see if you are entitled to help via a Disabled Facilities Grant:
England and Wales
https://www.gov.uk/apply-disabled-facilities-grant
Scotland
http://www.disabilityscot.org.uk/info-guides/disabled-home-adaptations-1/
Northern Ireland
https://www.nidirect.gov.uk/articles/disabled-facilities-grants-0
Republic of Ireland https://www.citizensinformation.ie/en/housing/housing_grants_and_schemes/housing_adaptation_grant_for_people_with_disability.html
If you are on a low income, or someone in your household is severely and permanently disabled, you may be entitled to a reduction in Council Tax. Further information is available in the Carers UK Council Tax factsheet: https://www.carersuk.org/images//Factsheets/2020-21_factsheets/Council_Tax_April_2020-21.pdf
Diet
During illness, nutritional needs are at their peak, but it is not unusual for patients to lose their appetites or taste for food. Worry and fear often accompany illness and can also contribute to loss of appetite. Good nutrition can be a powerful ally in the process of recovery, so if you need advice, ask to speak to a nutritionist. If taste has been affected, this will usually improve with time. Plastic utensils can be used if bitter or metallic tastes are experienced whilst eating. Sometimes taste changes can be related to medications, but drugs should not be discontinued without first consulting your GP. Try to eat a healthy, balanced diet and keep consumption of sugary and processed foods, and drinks that are high in caffeine or alcohol to a minimum. There is some excellent advice on nutrition on the NHS website; https://www.nhs.uk/live-well/eat-well/
Your immune system
Although caused by your immune system malfunctioning, CIDP does not weaken or damage your immune system, and having CIDP does not mean that your immune system is compromised, unless you are being treated with steroids.
Regular exercise and maintaining a healthy diet and sleep regime will all help during recovery. There is anecdotal evidence, and lots of hype surrounding supplements and alternative remedies, but very few are known to have real benefits. Most people are able to get the vitamins they need from their diet, but if you wish to take dietary supplements, your doctor (rather than Google!) will be able to advise you on anything that may help you during recovery.
Exercise and rest
Physiotherapy, occupational therapy (OT) and speech and language therapy play a vital role in maximizing functional ability.
Exercise can help to improve your muscle strength and reduce your overall sense of fatigue. It can also aid sleep and support mood through the production of endorphins. Other benefits include helping your heart and lungs remain healthy and making you feel more positive about yourself. However, it may take weeks or even months before you feel some of the benefits, so it is important to pace yourself. You will find lots of exercises online, including seated exercises, or you could ask your GP or physiotherapist about how to start regular exercise and what exercises might be right for you.
Visit the NHS website for advice on exercise: https://www.nhs.uk/live-well/exercise/
and also for advice on sleep: https://www.nhs.uk/live-well/sleep-and-tiredness/
Pain
Being in pain naturally impacts on mood and the ability to cope with everyday situations. If you are experiencing pain, it is important to talk to your family and friends about this, so that they understand what you are going through and why you might be irritable and difficult to live with at times.
Some other sources of support are shown below.
|
Other sources of support PAIN
|
|
| Pain Concern |
|
| British Pain Society |
https://www.britishpainsociety.org/
|
|
Pain Association Scotland
|
https://painassociation.co.uk/ |
| Welsh Pain Society |
https://www.welshpainsociety.org.uk/
|
| Pain Relief Foundation |
https://painrelieffoundation.org.uk/
|
| Pain Management NI |
https://www.myni.life/pain-management
|
| Pain Relief Ireland |
|
Mental health & wellbeing
With all the changes in your health it is not uncommon to feel anxious or angry, and this can even be helpful to a degree in providing the mental and physical energy that is needed to anticipate and tackle problems. An acute stress reaction is recognised as being a normal part of the process of adjusting to a life change, and it can often help to talk things through with a partner or close friend. However, please seek advice and help from your GP if you are finding it difficult to cope or to sleep, or if you are feeling overwhelmed emotionally.
The impact of being severely affected by a sudden, frightening and potentially life-changing condition such as CIDP can leave people with symptoms of PTSD (post-traumatic stress disorder). It can develop immediately, or many months or even years after a traumatic event. If you are concerned about low mood, irritability, panic attacks, anxiety, flashbacks, physical sensations such as trembling or sweating, poor concentration or sleeping problems, please talk to your GP about getting some counselling.
Some other sources of support are shown below.
|
Other sources of support MENTAL HEALTH
|
|
|
5 steps to mental wellbeing |
https://www.nhs.uk/conditions/stress-anxiety-depression/improve-mental-wellbeing/ |
| Mindfulness | https://bemindful.co.uk/ |
| Post-Traumatic Stress Disorder | https://www.nhs.uk/conditions/post-traumatic-stress-disorder-ptsd/ |
|
Mental health and wellbeing |
https://www.nhs.uk/conditions/stress-anxiety-depression/ |
| MIND | http://www.mind.org.uk/ |
| Young Minds | https://youngminds.org.uk/ |
Sexual relationships
CIDP and other chronic neuropathies can bring on problems in any relationship, and sexual relationships are not excluded. Dealing with a long-term illness or disability can put a great strain on a relationship, particularly when one partner is partially or totally dependent on the other. As well as coming to terms with a physical disability, the emotional upheaval can interfere with a couple’s sex life and this can be difficult to talk about. This can mean that the once close, intimate relationship can become distant and stressful for both partners. Help is available so speak to your GP or a relationship counsellor.
Other sources of relationship support
Relate: https://www.relate.org.uk/
Sexual Advice Association: https://sexualadviceassociation.co.uk/
Getting back to work
When someone is ready to return to work after an absence, the employer should have a procedure they follow. You can check your workplace’s absence policy for this. Your workplace might have a policy for meeting with employees after absences.
After long-term absence
If there’s been a long absence or the employee has an ongoing health condition, it’s a good idea for the employer and employee to meet and:
• make sure the employee is ready to return to work
• talk about any work updates that happened while they were off
• look at any recommendations from the employee’s doctor
• see if they need any support
• if the employee has a disability, see if changes are needed in the workplace to remove or reduce any disadvantages (‘reasonable adjustments’)
• consider a referral to a medical service such as occupational health
• discuss an employee assistance programme (EAP) if it’s available
• agree on a plan that suits you both, for example a phased return to work
Making reasonable adjustments
If an employee has a disability, by law their employer must consider making ‘reasonable adjustments’ if needed to help them return to work.
Reasonable adjustments could include making changes to the employee’s:
• workstation or working equipment
• working hours
• duties or tasks
This can help:
• get people back to work quicker
• prevent any further problems
For the best course of action, the employer should take advice from:
• the employee themself
• the employee’s doctor
• their occupational health adviser
Phased return to work
A ‘phased return to work’ is when someone who’s been absent might need to come back to work on:
• reduced hours
• lighter duties
• different duties
For example, after a:
• long-term illness
• serious injury
• bereavement
The employer or their HR manager and the employee should agree on a plan for how long this will be for.
For example, they could agree to review how things are going after a month and then decide to increase the working hours or duties, or they might decide they need to stay reduced for longer.
The employer or HR manager should continue to regularly review the employee’s health and wellbeing in the workplace and make new adjustments if necessary.
Pay during a phased return to work
If the employee returns to their normal duties but on reduced hours, they should get their normal rate of pay for those hours they work.
For the time they’re not able to work, they should get sick pay if they’re entitled to it.
If the employee is doing lighter duties, it’s up to the employer and employee to agree on a rate of pay. It’s a good idea to make sure this agreement is put in writing.
31
This information is provided by ACAS (the Advisory, Conciliation and Arbitration Service).
Further information regarding absence and returning to work is available on the ACAS website:
https://www.acas.org.uk/absence-from-work
Advice for carers
Hospital discharge can bring mixed emotions. Of course you’re glad to have your family member home, but it is quite normal to feel a bit daunted by what lies ahead, especially if you are now the main carer. Here are a few practical suggestions that can help you in your new role. Other sources of support are listed overleaf.
Ask for a needs assessment for the person you’re caring for – You need this before the council can recommend services such as equipment, home adaptations, help from a paid carer, etc
Get a carer’s assessment – This can be requested at the same time as a needs assessment, via social services at your local council
Don’t be afraid to ask for help – Ask family and friends (shopping, respite, etc), and contact carers’ organisations or Citizens Advice for benefits advice and other support
Look after yourself – Eat a healthy diet, maintain a regular sleep pattern and make time for exercise, preferably in the fresh air or at your local gym or pool, away from the care setting
Remember to rest – Put some activities on hold. Take some time to yourself by arranging respite care from a friend or relative or through social services
Recognise limitations – Both those of the person you’re caring for and your own. Let them try to do things for themselves if they are able, but bear in mind their safety and yours.
Look after your mental health – Talk to each other about your experiences and frustrations during illness and recovery. Talk to your GP if either of you is struggling
Be mindful of risks – Be aware of temperature (cooker, iron, hot bath water, hot drinks), risk of falls due to poor balance, and dropping or spilling things due to weakness
Diet & exercise – If appetite and taste are affected, ask about vitamin supplements to help maintain dietary needs. Ask the community physio about exercises to do between visits
Don’t lose sight of your relationship – Whatever your relationship is to the person you’re caring for, make time for it. Do things together that you both enjoy and that feel ‘normal’
Get in touch with GAIN – We provide information and support, organise peer support via phone or video link, virtual group chats, and run an active and supportive Facebook group
Other sources of support
| NHS advice | https://www.nhs.uk/conditions/social-care-and-support-guide/support-and-benefits-for-carers/ |
| Carers UK | https://www.carersuk.org/ |
| Carers Scotland | https://www.carersuk.org/scotland |
| Carers Wales | https://www.carersuk.org/wales |
| Carers Northern Ireland | https://www.carersuk.org/northernireland |
| Family Carers Ireland | https://familycarers.ie/ |
| Carers Trust | https://carers.org/ |
| Help for young carers | https://youngminds.org.uk/find-help/looking-after-yourself/young-carers/ |
| Citizens Advice UK | https://www.citizensadvice.org.uk/ |
| Citizens Information RoI | https://www.citizensinformation.ie/en/ |
| Find your local
social services |
England
https://www.nhs.uk/service-search/other-services/
Scotland https://www.mygov.scot/find-your-local-council/
Wales https://111.wales.nhs.uk/localservices/
Northern Ireland http://online.hscni.net/social-services/
Republic of Ireland https://www.hse.ie/eng/services/list/4/ |
